
A tonometer refers to the equipment that is used in tonometry – a test that measures the pressure inside your eyes, also known as intraocular pressure or IOP for short. Tonometry is rarely performed at your average comprehensive eye exam unless you are at high risk of or have been already diagnosed with glaucoma. Fortunately, tonometry can be used to detect changes in eye pressure before they cause any symptoms, enabling prompt action to be taken before your vision is affected.
About Glaucoma
Glaucoma is a common eye condition that occurs when the optic nerve, which connects the eye to the brain, becomes damaged. It’s normally caused by fluid building up in the front part of the eye, which causes the pressure inside the eyes to build. As the pressure increases, the optic nerve becomes increasingly damaged, and this prevents messages from being transmitted between your eyes and brain effectively. As a result, the patient’s vision becomes compromised. Without treatment, the level of vision loss will continue to increase. Unfortunately, any vision that has been lost as a result of glaucoma cannot be restored.
Most of the time, glaucoma develops very slowly which means that many people don’t realize that they are affected until some damage to their vision has already occurred. However, occasionally glaucoma can develop quickly, and symptoms do occur.
These can include:
Red eyes
Intense headaches
Tenderness around the eyes
Eye pain
Seeing rings/halos around lights
Blurred vision
Nausea and vomiting
If you notice any of these symptoms, it’s important that you make an appointment with your eye doctor right away so that you can be assessed. You are likely to have a tonometry test as part of this assessment.
What to expect from tonometry testing
There are various methods of tonometry testing, but many eye doctors use either Goldmann tonometry, which is the conventional technique to measure eye pressure, or electronic tonometry.
Goldmann tonometry testing is carried out using the Goldmann applanation tonometer, which is attached to a slit lamp microscope. This requires anesthetic eye drops to be used which numb your eyes, before a small probe is pressed gently against the eye, indenting the cornea. The pressure that the cornea pushes back onto the tonometer is what is measured to give your IOP reading. Electronic tonometry is where a handheld, mobile device is gently and quickly applied to the cornea to check the pressure, providing an accurate reading. Some eye doctors also offer non-contact tonometry which is where a puff of air is used to flatten the cornea, although this is reported to be less accurate than the Goldmann technique.
If you would like to find out more about Tonometry testing, please call our office to speak with our dedicated eyecare professionals.

In the ever-evolving world of vision correction, multifocal contact lenses have emerged as a game-changer for individuals seeking a seamless solution to address their presbyopia. As you navigate through life's various stages, your eyes may undergo changes that can impact your ability to focus clearly on objects at different distances. Multifocal contact lenses offer a convenient and effective way to combat this challenge, providing you with a versatile and comfortable option for correcting your vision.
What Are Multifocal Contact Lenses?
Multifocal contact lenses are specialized lenses designed to correct presbyopia, a condition that typically occurs as you age, making it difficult to focus on near objects. Unlike traditional single-vision lenses that correct either near or distance vision, multifocal contact lenses incorporate multiple prescriptions into a single lens. This innovative design allows you to enjoy clear vision at various distances, eliminating the need for separate reading glasses or bifocals.
How Do Multifocal Contact Lenses Work?
Multifocal contact lenses employ advanced optical technologies to provide seamless vision correction. These lenses feature distinct zones or concentric rings that correspond to different prescriptions for near, intermediate, and distance vision. As your eyes move and focus on objects at varying distances, the appropriate zone of the lens comes into play, ensuring a clear and comfortable visual experience.
There are two main types of multifocal contact lens designs:
Simultaneous Vision Design: In this design, the lens incorporates multiple prescriptions simultaneously, allowing your eyes to utilize the appropriate zone based on the viewing distance. This design can take some time to adjust to, as your brain learns to interpret the different visual inputs.
Alternating Vision Design: Also known as "segmented" or "translating" lenses, these lenses have distinct zones for near and distance vision. As you move your eyes or shift your gaze, the appropriate zone is positioned in front of your pupil, providing the necessary correction.
Eye Conditions That Multifocal Contact Lenses Can Treat
Multifocal contact lenses are primarily designed to address the following vision-related conditions:
Presbyopia: As you age, the natural lenses in your eyes lose flexibility, making it challenging to focus on nearby objects. Multifocal contact lenses can correct this age-related farsightedness, allowing you to see clearly at all distances.
Myopia (Nearsightedness): If you struggle to see distant objects clearly, multifocal contact lenses can incorporate a prescription to correct myopia, while also providing near and intermediate vision correction.
Hyperopia (Farsightedness): For individuals with farsightedness, multifocal contact lenses can offer a solution by incorporating a prescription to improve distance vision, along with near and intermediate vision correction.
Astigmatism: Some multifocal contact lenses are designed to correct astigmatism, a condition caused by an irregularly shaped cornea or lens, resulting in blurred or distorted vision.

Cataracts are a common eye condition that can significantly affect your vision. They occur when the lens of your eye becomes cloudy, causing blurred or distorted vision. This clouding is typically a result of aging, but other factors such as genetics, diabetes, or prolonged exposure to sunlight can also contribute to the development of cataracts.
As cataracts progress, you may experience symptoms such as difficulty seeing at night, increased sensitivity to glare, or a decrease in color perception. These changes can make daily activities like reading, driving, or recognizing faces more challenging.
Why Cataract Surgery May be Necessary
Cataract surgery is often recommended when cataracts start to interfere with your vision and affect your ability to perform daily tasks. The primary goal of cataract surgery is to remove the cloudy lens and replace it with an artificial intraocular lens (IOL).
The decision to undergo cataract surgery is a personal one and should be made after consulting with your optometrist. Factors such as the severity of your cataracts, your overall eye health, and your lifestyle requirements will be taken into consideration when determining if surgery is necessary.
What is Cataract Surgery Co-Management?
Cataract surgery co-management refers to the collaborative approach between an ophthalmologist, who performs the surgery, and an optometrist, who provides pre-operative and post-operative care. This partnership ensures that you receive comprehensive eye care throughout the entire process, from the initial consultation to the final follow-up appointments.
Your optometrist plays a crucial role in cataract surgery co-management by conducting a thorough pre-operative evaluation to assess your overall eye health and determine the most suitable IOL for your specific needs. They will also provide guidance and education on the surgical procedure, address any concerns you may have, and help you make informed decisions about your eye care.

If you have recently undergone eye surgery, your eye doctor may recommend the use of post-surgical contact lenses as part of your recovery process. These specialized lenses are designed to aid in the healing and protection of your eyes after surgery.
Why Post-Surgical Contact Lenses May Be Necessary
After eye surgery, your eyes are in a delicate state and require extra care to ensure proper healing. Post-surgical contact lenses can play a crucial role in this process. These lenses act as a protective barrier, shielding your eyes from irritants such as dust, debris, and bright lights. They also help to maintain the shape of the cornea and aid in the prevention of infection. By wearing post-surgical contact lenses, you can minimize the risk of complications and promote a faster and smoother recovery.
Different Types of Post-Surgical Contact Lenses
There are various types of post-surgical contact lenses available, and the specific type recommended for you will depend on the nature of your surgery and your eye condition. One common type is the bandage contact lens, which is a soft, therapeutic lens that covers the cornea, providing protection and promoting healing.
Another type is scleral lenses, which is larger and covers a larger portion of the eye, providing enhanced protection and support. Your optometrist will determine the most suitable type of post-surgical contact lens for your individual needs.

Contact lenses have become a popular choice for individuals who want to correct their vision without the hassle of wearing glasses. Traditional contact lenses have been around for decades, offering a convenient alternative to eyeglasses. However, advancements in technology have given rise to a new type of contact lens – hybrid contacts.
What Are Hybrid Contacts?
Hybrid contacts are a revolutionary type of contact lens that combine the best features of both soft and rigid gas permeable (RGP) lenses. The rigid center corrects vision by providing precise clarity, while the soft skirt offers comfort and stability. This unique combination allows for the benefits of both types of lenses to be experienced simultaneously.
The central RGP lens of a hybrid contact is made from a rigid material that allows oxygen to pass through to the cornea, ensuring ample oxygen supply to the eyes. This ensures the overall health of the eyes, preventing dryness and reducing the risk of complications associated with limited oxygen flow

Colored contacts have become increasingly popular over the years as a way to enhance your look and experiment with different eye colors. Whether you want to change your eye color for a special occasion or simply for everyday wear, colored contacts offer a fun and versatile option.
Different Types of Colored Contacts
When it comes to colored contacts, there are various types to choose from, depending on your preferences and needs. The three main categories are cosmetic, enhancement, and opaque lenses.
Cosmetic lenses are designed to completely change the color of your eyes. These lenses come in a wide range of shades, from natural hues such as blue, green, and brown, to more vibrant colors like purple, gray, and even red. Cosmetic lenses can create a dramatic transformation and give you the eye color you desire.
Enhancement lenses, on the other hand, are designed to enhance your natural eye color rather than change it completely. They add depth and intensity to your eyes, making them appear brighter and more vibrant. Enhancement lenses are ideal if you want a subtle change that enhances your natural beauty.
Opaque lenses are specifically designed to cover dark-colored eyes. They are ideal for individuals with naturally dark eyes who want to achieve a lighter or more vibrant eye color. Opaque lenses are often used in theatrical or costume applications as they can create a striking and captivating look.

If you find it difficult to tell colors apart, you may be color blind. Color blindness, or color deficiency, is estimated to affect around 8% of men and about 1% of women, but for those affected, it can significantly impact the quality of their day-to-day life. Contrary to popular belief, being color blind doesn’t mean that you can’t see any color at all. Instead, patients simply struggle to differentiate between certain colors. The vast majority of people who are color blind find it impossible to tell the difference between varying shades of red and green. You may hear this referred to as red-green color deficiency. However, this doesn’t only mean that they mix up red and green. They can also mix up colors that have some green or red light as part of their whole colors, for example purple and blue. This is because they are unable to see the red light that forms part of the color purple.
As you can probably imagine, this type of visual impairment can be a problem for things like traffic lights, taking medications and even looking at signs and directions. For example, someone who is color blind may find that the green on a traffic light may appear white or even blue.
EnChroma lens technology is specifically designed to counteract red-green color deficiency and enable patients to better identify the difference in these colors or shades. They do this by selectively filtering out the red and green wavelengths of light at the exact point where the color sensitivities overlap before hitting the retina, creating far greater contrast between the colors so that the patient can distinguish between them successfully. Most cases of color blindness respond well to EnChroma’s innovative spectral lens technology, giving patients the ability to experience life in bright, vibrant technicolor.
EnChroma lenses are made from leading edge, Trivex material, and this helps to give them the best possible quality and clarity of vision. These lenses are also extremely light, strong and offer patients 100% protection against UV light, helping to keep your eyes healthy as well as improving your vision.
If you or someone you know is color blind or color deficient and could benefit from EnChroma lenses, contact us today to learn more about how they can help!
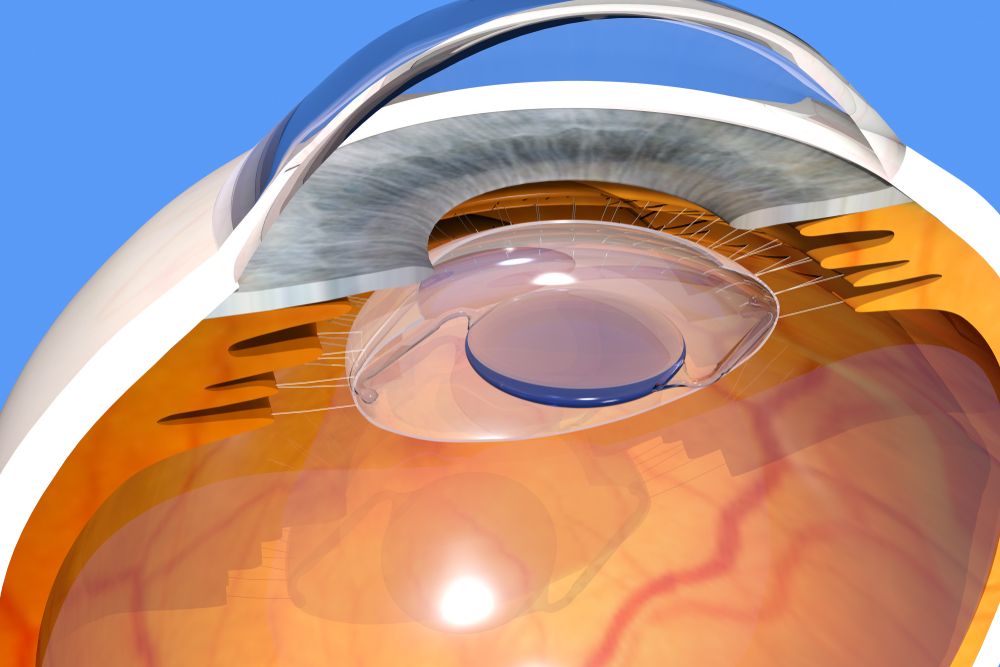
Clear Lens Extraction (CLE) is a surgical procedure that involves the removal of the natural lens of the eye and replacing it with an artificial lens implant, also known as an intraocular lens (IOL). CLE is primarily performed to correct refractive errors, such as nearsightedness, farsightedness, and astigmatism.
Understanding CLE and How It Works
Clear Lens Extraction is similar to cataract surgery, where the natural lens is removed and replaced with an IOL. However, in CLE, the lens is clear and not clouded as in the case of cataracts. The procedure begins with the administration of local anesthesia to numb the eye and ensure a painless experience for the patient.
Once the eye is numb, a small incision is made on the cornea, which is the clear front surface of the eye. Through this incision, your eye surgeon accesses the lens and carefully removes it. The artificial IOL is then inserted into the empty lens capsule. The IOL is specifically chosen to correct the patient's refractive error, providing them with improved vision.
After the IOL is implanted, the incision is closed with tiny sutures or self-sealing techniques. Following the surgery, patients are usually prescribed antibiotic and anti-inflammatory eye drops to prevent infection and reduce inflammation.
Factors to Consider Before Undergoing Clear Lens Extraction
Before deciding to undergo Clear Lens Extraction, there are several factors that need to be considered. Firstly, it is crucial to have a thorough eye examination to determine if you are a suitable candidate for the procedure. Your optometrist will evaluate your overall eye health and discuss your expectations and goals for vision correction.
Age is another important factor to consider. CLE is typically recommended for individuals over the age of 40 who have developed presbyopia, a condition that affects near vision. It is also important to have stable vision, as any changes in prescription can affect the accuracy of the IOL power calculation.
Additionally, it is essential to understand the potential risks and complications associated with the procedure. While CLE is generally safe, there is a small risk of infection, bleeding, and retinal detachment. Your optometrist will discuss these risks with you and address any concerns you may have.

Thanks to the advancement of lens technology, glasses lenses are no longer a single, one size fits all solution. There are a variety of different lens types that can be used in glasses, giving patients greater flexibility and control over their vision than ever before.
Single Vision Lenses
Also known as monovision lenses, these lenses are designed to correct the wearer’s vision at just one distance, and have a single prescription covering the entire surface of the lens. They are most often recommended for people who are either nearsighted (myopia) or farsighted (hyperopia) and who need glasses for a specific activity, such as driving or reading.
Progressive Lenses
Progressive lenses are multifocal lenses that can correct a patient’s vision at different working distances, ranging from far distance to reading distance. However, rather than designating different areas on the lenses for different distances with visible lines separating them, progressive lenses have a gradual change so that the wearer can smoothly transition from one lens power to another.
Bifocal and Trifocal Lenses
As you may have guessed from the name, bifocal and trifocal lenses have either two or three lens powers depending on which type you choose. Bifocal lenses support distance vision in the top half of the lens, and near vision in the lower half. Trifocal lenses support distance vision in the top third of the lens, intermediate vision in the middle segment and near vision in the bottom third. Whichever variety you choose, you will see visible lines separating each segment.
Bifocal and trifocal lenses are recommended for patients who are near or farsighted, and those who develop presbyopia, which is the natural hardening of the eye lens, that occurs as we get older. Presbyopia makes it harder for the lens of the eye to adapt to focus at different distances.
Multifocal Lenses
Multifocal lenses are the alternative name given to bifocal, trifocal and progressive lenses.
Computer Lenses
Computer lenses are prescription lenses that are specifically designed to be worn when doing computer work. This is because they place the optimum lens power for viewing your computer screen exactly where you need it – which is closer than intermediate vision, but further away than reading material is usually held. Wearing computer lenses can significantly reduce the negative effects caused by the high visual demands of computer work, including blurred vision, redness, dry eyes, double vision and dizziness.
Transition Lenses
Also known as photochromic lenses, transition lenses are a special type of lens that darken when in the sunlight and lighten when in softer light or the dark. This versatility gives the wearer the convenience of being able to move between different environments without needing to change their glasses. This makes them extremely cost effective and prevent the wearer from needing to take multiple pairs of glasses out with them. Transition lenses also filter out many of the harmful UV rays that are emitted from the sun, helping to keep eyes healthy too. They are ideal for people who spend a lot of time going between inside and outside, or who work outside in varying weather conditions.
Blue Light Lenses
Blue light lenses are specially crafted lenses that contain filters that block out much of the artificial blue light that is produced by digital devices like computers, smartphones and tablets. Natural blue light is actually good for balancing our sleep-wake cycle, boosting our mood and enhancing our cognitive abilities so that we can function better day to day. However, too much blue light, especially from artificial sources, can have the opposite effect. Many people who fail to use blue light lenses can go on to develop digital eye strain, which produces symptoms like eye fatigue, dry eyes, blurred vision, headaches and more. Blue light lenses are recommended for anyone who spends a lot of time working on a digital device.
Polarized Lenses
Polarized lenses are used to reduce eyestrain and improve the quality of vision in patients on especially sunny days, making them ideal for anyone who spends a lot of time outdoors. They can do this because they have a special filter that blocks some of the light from passing through the lens. Vertical light is allowed to pass through, while horizontal light, such as that which bounces off of water and can be blinding, is blocked. Polarized lenses are most often used in sunglasses since they are worn outdoors, and the wearer also needs to protect their eyes from UV damage.
Still have questions about which lens is right for you? Contact us to schedule an eye exam or an appointment to evaluate your individual needs.

Dry eye is a common ocular condition that occurs when the eyes do not produce enough tears or when the tears evaporate too quickly. This can lead to discomfort, redness, blurred vision, and even damage to the surface of the eyes. Understanding the causes and symptoms of dry eye is crucial provide early detection and effective treatment.
The Importance of Dry Eye Advanced Diagnostic Testing
Early detection of dry eye is crucial for preventing further progression of the condition and improving patient outcomes. Without proper diagnosis and treatment, dry eye can cause significant discomfort and affect daily activities. Additionally, chronic dry eye can lead to corneal ulcers, infections, and even vision loss. By accurately identifying and addressing dry eye in its early stages, optometrists can provide timely interventions and prevent complications.
TearLab
One of the advanced diagnostic tools available for dry eye is TearLab. TearLab is a non-invasive test that measures the osmolarity of tears, which is an indicator of tear film stability. This test provides valuable information about the quality and quantity of tears, allowing healthcare professionals to accurately diagnose and monitor dry eye. By analyzing the osmolarity of tears, TearLab helps identify the severity of dry eye and guides treatment decisions. It is a quick and painless procedure that can be performed in a clinical setting.
InflammaDry
Inflammation plays a significant role in dry eye, and identifying the presence of inflammation is crucial for effective treatment. InflammaDry is a diagnostic tool that detects elevated levels of matrix metalloproteinase 9 (MMP-9), an inflammatory marker, in tears. By measuring MMP-9, InflammaDry helps optometrists differentiate between inflammatory and non-inflammatory dry eye. This information is essential for tailoring treatment plans and determining the most appropriate therapies for each patient.








